Analysis of 1990-2021 data shows wider access to antibiotics and better treatment could save 92 million lives by 2050.
By 2050, approximately 2 million people — predominantly over 70 — could die each year due to drug-resistant infections, according to a global analysis of antimicrobial resistance published in “The Lancet”.
The report estimates over 39 million deaths from antibiotic-resistant infections between now and 2050. It highlights that more than 1 million people die annually from such infections, a figure that could nearly double by mid-century.
The analysis, which examines data from 1990 to 2021, suggests that wider access to appropriate antibiotics and improved infection treatment could save 92 million lives between 2025 and 2050. “This report provides a crucial understanding of how we arrived at this point and gives a realistic expectation of the future burden of resistance,” commented Joseph Lewnard, an epidemiologist at the University of California, Berkeley.
Timothy Walsh, a microbiologist at the University of Oxford, notes that the real burden could be higher due to data gaps in many regions. The findings indicate that the global effort is falling short of the UN’s target to reduce antimicrobial resistance (AMR)-related deaths by 2030.
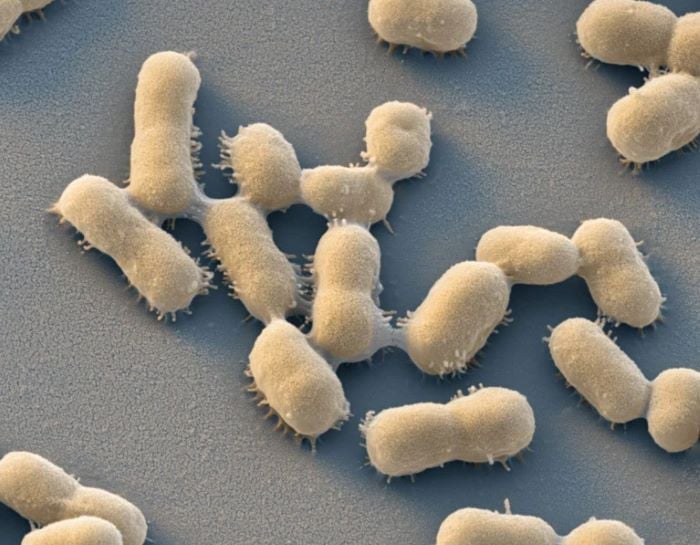
Key findings reveal that while deaths in children under five from drug-resistant infections have decreased by 50% in the past 30 years, mortality among those aged over 70 has surged by 80%. The deadliest infections are largely caused by gram-negative bacteria, which are highly resistant to Carbapenem antibiotics. Deaths from these bacteria have risen by 149%, with 127,000 deaths recorded in 2021.
The report warns that by 2050, AMR could lead to 1.91 million deaths annually, with an additional 8.22 million people dying from resistance-related illnesses. More than 65% of these deaths will affect those over 70. Co-author Mohsen Naghavi stresses the need to address healthcare quality and infection prevention.
Researchers urge that strategies focus on regions like South Asia, Latin America, and the Caribbean, with a particular emphasis on supporting low- and middle-income countries. Timothy Walsh advocates for increased global investment, ensuring access to antibiotics, clean water, and sanitation in lower-income areas. He also calls for a reduction in antibiotic overuse in farming and greater investment in research for new drugs and vaccines.
The authors hope the report will help guide the development of innovative treatments and preventive measures against the growing threat of antimicrobial resistance.


